Undernutrition and severe acute malnutrition in children
BMJ 2017; 359 doi: https://doi.org/10.1136/bmj.j4877 (Published 16 November 2017) Cite this as: BMJ 2017;359:j4877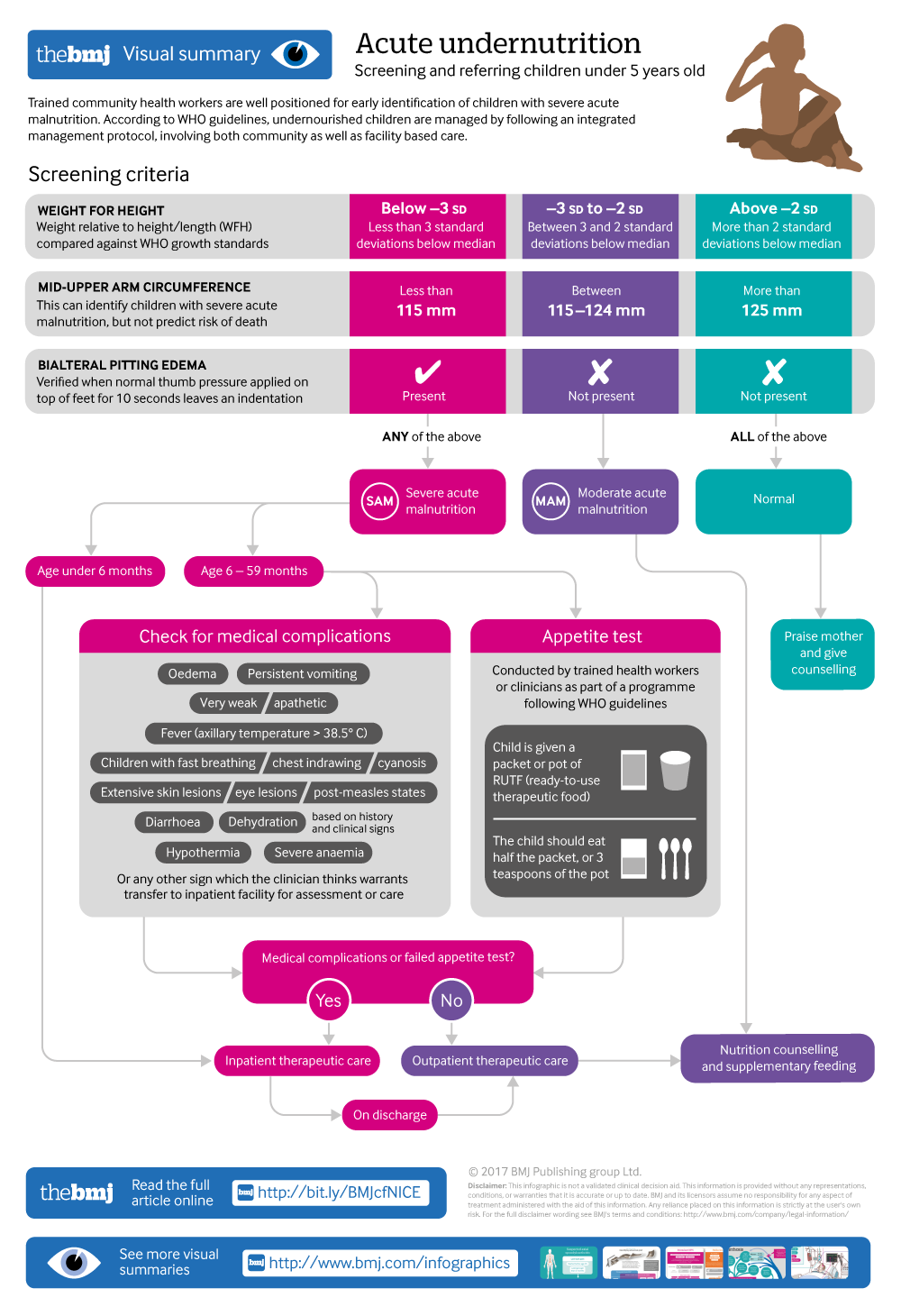
Infographic available
Click here for a visual overview of screening and referring children under 5 years old with acute undernutrition
- Suparna Ghosh-Jerath, additional professor1,
- Archna Singh, associate professor2,
- Nameet Jerath, senior consultant3,
- Suruchi Gupta, research assistant1,
- Elizabeth F Racine, professor4
- 1Public Health Foundation of India, Indian Institute of Public Health-Delhi, Gurgaon, Haryana 122002, India
- 2Biochemistry Department, All India Institute of Medical Sciences, New Delhi, India
- 3Indraprastha Apollo Hospital, Pediatrics, New Delhi, India
- 4Department of Public Health Sciences, University of North Carolina at Charlotte, Charlotte NC, USA
- Correspondence to: S Ghosh-Jerath suparna.ghoshj{at}iiphd.org
What you need to know
Children with moderate to severe acute malnutrition have three to nine times higher mortality than well nourished children
In areas with high rates of undernutrition, assess nutritional staus of all children under 5 years old using standard anthropometric measures
Refer children with medical complications, oedema, or poor appetite to a medical centre for inpatient management with standard feeding protocols
Children who are well and alert can be managed in the community with optimal diet, counselling mothers about child care and feeding, and regular follow-up
The choice between ready-to-use therapeutic foods or home prepared food must be guided by local availability, costs, and caregiver preferences
Undernutrition contributes to nearly 45% of all deaths in children under 5 years old globally.1 Low and middle income countries are worst affected.2 Treatment services are estimated to reach less than 15% of undernourished children.3 Healthcare providers can play a crucial role in identifying undernutrition in children and ensuring appropriate care and referral.
We provide an overview of assessment and initial management of undernutrition in children under 5 years of age. For the purpose of this paper, we focus on severe acute malnutrition, when children are at increased risk of medical complications unless diagnosed and managed promptly.
What encompasses child undernutrition and severe acute malnutrition?
Undernutrition results from insufficient intake of energy foods (carbohydrates, fats), proteins, and micronutrients (vitamins and minerals).4 Energy and protein malnutrition can manifest clinically as marasmus, kwashiorkor, and marasmic-kwashiorkor (see fig 1⇓ and fig 2⇓). The current World Health Organization guidelines subsume these entities into the blanket term “severe acute malnutrition,” and its variants with or without medical complications.5 Acute malnutrition results from hunger or disease, or both, and is associated with rapid weight loss or failure to gain weight. Box 1 outlines the subclinical and clinical forms of undernutrition. Iron, iodine, vitamin …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £184 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£50 / $60/ €56 (excludes VAT)
You can download a PDF version for your personal record.
