Zika virus: management of infection and risk
BMJ 2016; 352 doi: https://doi.org/10.1136/bmj.i1062 (Published 26 February 2016) Cite this as: BMJ 2016;352:i1062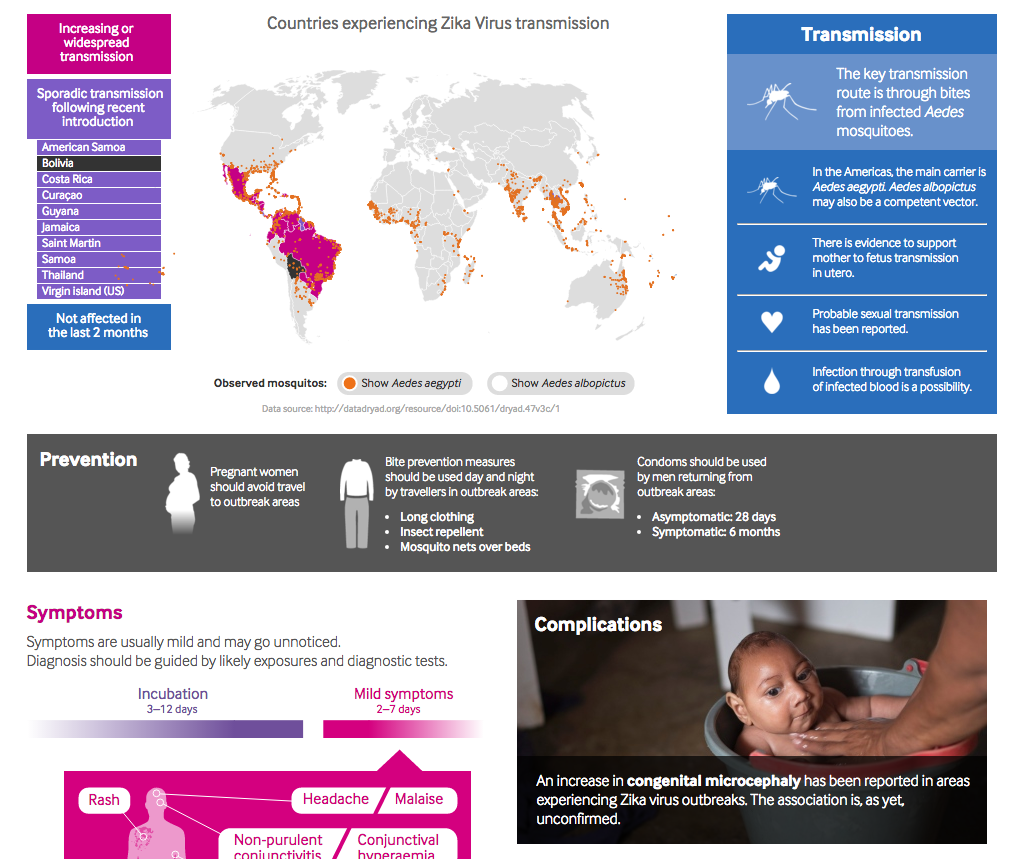
Zika: A clinical guide
See a quick overview of the key facts, including countries affected, and advice on prevention, diagnosis and management of patients returning from outbreak areas.

Brazilian Portugese translation
Vírus da Zika: manejo da infecção e do risco
- Shazaad S Y Ahmad, specialty trainee in infectious diseases and virology1 2,
- Tejal N Amin, clinical research fellow and specialty trainee in obstetrics and gynaecology3,
- Andrew Ustianowski, consultant in infectious diseases1
- 1Northwest Regional Infectious Diseases Unit, North Manchester General Hospital, Pennine Acute Hospitals Trust, Manchester M8 5RB, UK
- 2Virology Department, Manchester Royal Infirmary, Central Manchester Foundation Trust, Manchester Academic Health Sciences Centre, Manchester M13 9WL, UK
- 3Department of Obstetrics and Gynaecology, University College London Hospitals NHS Foundation Trust, London, UK
- Correspondence to: A Ustianowski Andrew.Ustianowski{at}pat.nhs.uk
AMI IMAGES / SPL
What you need to know
-
Zika virus produces a mild illness with non-specific symptoms and may be symptomatic in just one in four cases
-
The link between infection in pregnancy and microcephaly is not fully characterised
-
Offer pregnant women at risk of infection a monthly fetal scan, and discuss those with symptoms with an infectious disease specialist
-
Women who are pregnant or planning pregnancy should consider avoiding travel to affected areas
-
Advise men returning from affected areas to avoid unprotected sex with female partners of childbearing potential for 28 days, and for six months if they have probable or confirmed infection
Zika virus has caused a self limiting pyrexial illness from Africa to South-East Asia for decades. Recently it has spread across the Pacific and in 2015 caused infections for the first time in South America. Though usually asymptomatic or of little clinical significance in adults, there is concern about an apparent association between infection in pregnancy and birth defects such as microcephaly.1 2 3 We have no data to characterise the risks of abnormal fetal development and adverse pregnancy outcomes, or to guide testing strategies. In its absence, global health bodies have issued guidance for clinicians on how to minimise the risk of transmission to those who are, or may become, pregnant, and to monitor fetuses that may have been exposed.
We present current management advice for healthcare professionals in non-endemic countries, who may offer advice to individuals concerned about pregnancy and conception before or after travel to an area with Zika virus. Guidance is likely to change as the clinical picture and knowledge base develop, and up to date advice can be accessed from sources such as those listed in box 1.
Box 1: Sources of up to date advice on Zika virus and management of those exposed
-
Public Health England—www.gov.uk/guidance/zika-virus
-
Royal College of Obstetricians and Gynaecologists—www.rcog.org.uk/en/news/interim-clinical-guidelines-on-zika-virus-infection-and-pregnancy/
-
National Travel Health Network and Centre (NaTHNaC) for travel advice—http://travelhealthpro.org.uk/zika-virus-update-and-advice-for-travellers-including-pregnant-women/
-
Health Protection Scotland—www.hps.scot.nhs.uk/internationalissues/zika.aspx
-
European Centre of Disease Control—http://ecdc.europa.eu/en/healthtopics/zika_virus_infection/Pages/index.aspx
-
Centers for Disease Control and Prevention—www.cdc.gov/zika/
-
Australian Department of Health—www.health.gov.au/internet/main/publishing.nsf/Content/ohp-zika.htm
-
World Health Organisation—www.who.int/csr/disease/zika/en/
An accompanying article4 discusses the epidemiology and the evidence of what is currently known, including a possible association with Guillain–Barré syndrome.
Example scenario 1
A 27 year old woman has just returned from Colombia. While she was there she felt mildly unwell. Yesterday she discovered that she was pregnant and is anxious about whether she had Zika virus. She has heard that it will damage her baby’s brain.
Take a travel history from pregnant women concerned about, or at risk of, Zika virus infection, and from their male sexual partners. Box 2 lists countries where Zika virus is currently present, such as Colombia. There is no evidence to suggest that Zika virus poses a specific problem for maternal health.
Box 2: Countries with transmission of Zika virus as reported by the European Centre of Disease Control*
Increasing or widespread transmission
-
American Samoa
-
Barbados
-
Brazil
-
Cape Verde
-
Colombia
-
Curaçao
-
Dominican Republic
-
Ecuador
-
El Salvador
-
French Guiana
-
Guadeloupe
-
Guatemala
-
Haiti
-
Honduras
-
Martinique
-
Mexico
-
Nicaragua
-
Panama
-
Paraguay
-
Puerto Rico
-
Samoa
-
Suriname
-
Venezuela
-
Tonga
Sporadic transmission after recent introduction
-
Aruba
-
Bolivia
-
Bonaire
-
Costa Rica
-
Guyana
-
Jamaica
-
Saint Martin
-
Thailand
-
Virgin Islands (US)
Transmission in the past nine months but not in the past two months
-
Fiji
-
Maldives
-
New Caledonia
-
Solomon Islands
-
Vanuatu
-
*For up to date lists refer to ECDC (http://ecdc.europa.eu/en/healthtopics/zika_virus_infection/zika-outbreak/Pages/Zika-countries-with-transmission.aspx)
The risk of congenital abnormalities is poorly characterised
The risk of Zika virus infection to a developing fetus is not fully understood. The recent rise in such infections has coincided with an apparent increase in birth defects—predominantly microcephaly but also ventriculomegaly, cell migration abnormalities, congenital contractures, stillbirth, and neonatal death.2 5 These abnormalities have largely been described in case reports and case series. A direct causal link has not been confirmed, but there is evidence of Zika virus infection in placentas of aborted fetuses and in the brains of babies with microcephaly who died soon after birth.6 7 If causality is established, further data will be needed before we could tell a pregnant woman how likely it is that she would have an affected child.
Preliminary data from a small case series suggest that infection in the early stages of pregnancy may pose the greatest risk,5 consistent with other viral infections such as rubella. No treatment is presently available to correct or alter the chances of adverse fetal outcomes.
Testing and monitoring of pregnant women is guided by symptoms
There is an absence of good evidence to guide testing and monitoring. However, expert guidance has been issued by international bodies.
Figure 1⇓ shows UK guidance for pregnant women who have travelled to an area with known Zika virus transmission during the pregnancy.1 In essence, all pregnant women who have travelled to an area affected by Zika virus should be offered a baseline fetal ultrasound scan and should be discussed with a secondary care obstetric team. If the ultrasound is normal, offer scans every four weeks throughout the pregnancy. Microcephaly and the other neurological abnormalities described may not become apparent on scans until after 20 weeks’ gestation or into the third trimester. Logistically, testing and care may be led by obstetric teams or form part of joint care with midwives or primary care doctors.
Fig 1 Algorithm for assessing pregnant women exposed to Zika virus1
Detection of any neurological abnormalities, such as a small head (more than two standard deviations below the mean for gestational age) or intracranial calcifications, warrants referral to a fetal medicine unit for further investigation. Here, alternative causes of microcephaly—such as other congenital infections, chromosomal abnormalities and undefined genetic syndromes, exposure to teratogenic substances, and maternal metabolic diseases—will also be considered.
Pregnant women who present with clinical symptoms compatible with Zika virus infection (see box 3) while in, or within two weeks of return from, a Zika virus affected area should be considered for testing for Zika virus infection and other travel associated diseases relevant to the country of travel. Those who are asymptomatic but have just returned should be advised to seek medical care if they develop any symptoms consistent with Zika virus within the next two weeks.
Box 3: Clinical symptoms consistent with Zika virus infection1
Suspect Zika virus infection in those who have any of the following symptoms and relevant travel history:
-
Low grade fever
-
Arthralgia
-
Maculopapular rash (sometimes itchy)
-
Conjunctivitis
-
Headache
-
Myalgias
-
Eye pain
Interpreting tests for Zika virus is complicated
All patients undergoing testing for Zika virus infection should be discussed with infection specialists and the optimum testing strategy for this and any other infections agreed. The first line test and definitive diagnosis is made by identification of Zika virus RNA by means of PCR (polymerase chain reaction). This may remain detectable in blood for the first five days of infection and probably for up to two weeks in urine.8 Use the test in those with current or recent symptoms in liaison with the local virology laboratory. (In the UK this is generally serum and an EDTA blood sample, and also urine in sterile container if the patient is pregnant.)
If Zika virus RNA is detected, UK guidance suggests that the woman is offered direct referral to fetal medicine specialists. However, a negative PCR result cannot exclude infection (especially if the sample is sent several days after the onset of any symptoms), and follow-up with screening ultrasound scans at four-weekly intervals should be offered in this situation.
The United States uses a Zika virus IgM assay, and Australia is using IgM and IgG assays in an attempt to detect infections, including in those outside the testing window for viral RNA. The US Centers for Disease Control and Prevention advocates that all pregnant women returning from affected areas should be tested for Zika virus,9 with PCR tests if symptomatic and serological tests if asymptomatic.
The sensitivity, specificity, and applications of such serological tests (IgG or IgM) are not established, however. They are not currently advocated in the UK, although storage of a serum sample for potential future testing (once assays have been established and validated) may be suggested.
Amniotic fluid, if sampled, may also be tested by PCR, but the utility of such testing is not firmly established at present.
Example scenario 2
A 28 year old man has returned from Brazil and has flu-like symptoms. He is worried that he has Zika virus. He is not sure he should go to work. He has also heard that it can be sexually transmitted and is worried about his partner.
Discuss all those with symptoms and relevant travel history with local infection specialists
It is estimated that four out of five people with Zika virus infection are asymptomatic, and in those who do develop symptoms these are often non-specific (box 3). It is therefore important that the case of a symptomatic individual, such as described above, is discussed with a local infection specialist to allow assessment for other potential infections such as malaria and dengue.
Zika infection is not a notifiable disease in the UK, but it is in other countries such as the US and Australia.
Zika is transmitted via a type of mosquito but possibly also by semen or blood products
There is no need to avoid work or other activities of daily living. Zika virus is transmitted from human to human via a vector, the Aedes mosquitoes. These mosquitoes are not present in the UK, northern Europe, Canada, northwestern United States, Russia, northeastern Asia, and southern Australia, but they are widespread throughout much of the rest of the world.
It is possible that Zika virus may pass from human to human via other routes. There is a theoretical risk of transmission via infected blood or blood products.10 The virus has been identified in semen from two men infected with Zika virus,11 12 and, to date, there have been two reported instances of sexual transmission by male travellers to their partners in non-endemic areas (only one of these cases is presently published13). It is not known how long after infection the virus is detectable, or potentially infectious, in semen. There is no evidence of sexual transmission from women to men.
UK and European guidance advises that men with suspected or confirmed infection should use condoms with their partners (if pregnant or at risk of pregnancy) for six months.1 2 Abstaining would be another option. The US advises abstaining or using condoms for the duration of the pregnancy if the partner is pregnant, but does not specify a time period if they are not.14
For men who have been asymptomatic during travel in affected areas and for two weeks after return, UK and European guidance suggests that they consider using condoms for 28 days after their return if their partner is pregnant or at risk of pregnancy.1 2 The US guidelines do not specify a time period for asymptomatic men. The current advice is that condoms should be used for vaginal, oral, and anal sex. This should be discussed with patients.
These time periods are poorly evidence based. The 28 day window has been suggested to allow a 14 day incubation period and a 14 day viraemic period, even in asymptomatic people. The six month window may change once longer term data on seminal carriage is established.
Patients planning to donate blood, tissue, or semen should declare recent travel to affected areas (and Zika virus test results where known) before donation.
Example scenario 3
A 32 year old woman is planning to travel on a work trip to Brazil. She is not pregnant but is contemplating starting a family soon. She asks how long risks may persist and wonders how to minimise the chance of infection.
Risk to future pregnancies is unknown
There are few data to support advice on the duration of risk after potential exposure, but guidance has been issued. There is consensus across UK,1 European,2 US,3 and Australian15 guidance that women of childbearing potential who are travelling to Zika affected areas should ensure they are using reliable contraception and should avoid conceiving. Women who are pregnant should be strongly advised to avoid such travel if possible.
On return from endemic areas, advice in the UK is to avoid becoming pregnant for a further 28 days.1 It is thought, though with little evidence, that a fetus conceived after a woman has cleared the virus would not be at risk of birth defects, nor should there be any risks to future pregnancies.3 There is no known site of longer term carriage (such as in semen) in women.
Advise all travellers on how to avoid mosquito bites
If travel to an affected area is unavoidable, healthcare providers should fully inform the individual on avoidance of mosquito bites. Aedes mosquitoes bite from dawn through to dusk (only rarely at night), and 24 hour preventive measures should be encouraged. DEET based insect repellents should be used and applied frequently, and other measures should be pursued (see box 4).
Box 4: Mosquito bite avoidance
-
Wear long-sleeved shirts and long trousers
-
Stay in places that use window and door screens to keep mosquitoes outside or have closed windows and air conditioning
-
Sleep under a mosquito bed-net.
-
Use mosquito repellents that contain 50% DEET (N,N-diethyl-m-toluamide) (deemed safe in pregnancy)
-
Apply DEET after sunscreen
-
Treat clothing with permethrin or purchase permethrin treated items. See product information to determine how long the protection will last
-
Public Health England’s “Mosquito bite avoidance for travellers” information sheet is available from www.gov.uk/government/publications/mosquito-bite-avoidance-for-travellers
How were patients involved in the creation of this article?
The BMJ did not ask the authors to involve patients in the creation of this article.
Footnotes
-
Contributors: All authors contributed to drafts and revisions of the manuscript and approved the final version for publication. AU is the guarantor.
-
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
-
Provenance and peer review: Commissioned; externally peer reviewed.




