Zika virus
BMJ 2016; 352 doi: https://doi.org/10.1136/bmj.i1049 (Published 26 February 2016) Cite this as: BMJ 2016;352:i1049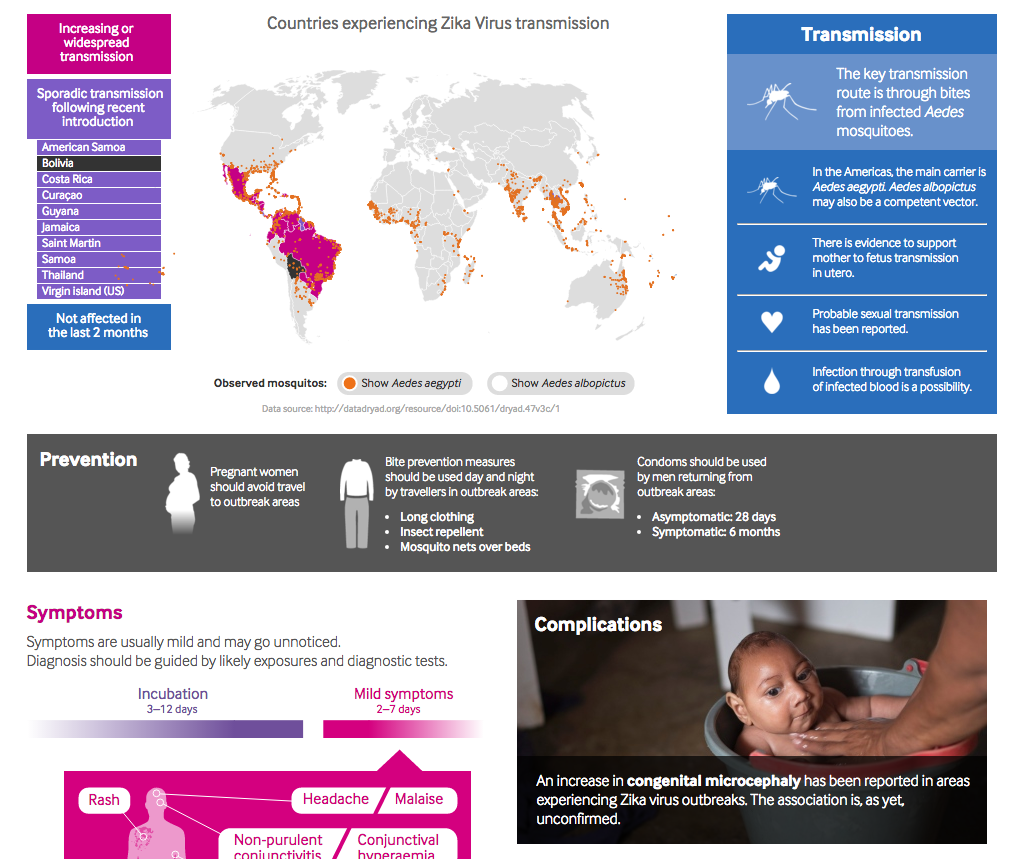
Zika: A clinical guide
See a quick overview of the key facts, including countries affected, and advice on prevention, diagnosis and management of patients returning from outbreak areas.

Brazilian Portugese translation
Vírus da Zika
- Marina Basarab, specialty registrar1,
- Conor Bowman, senior clinical fellow1,
- Emma J Aarons, consultant virologist and infectious diseases physician2,
- Ian Cropley, consultant infectious diseases physician1
- 1Department of Infectious Diseases, Royal Free London NHS Foundation Trust, London NW3 2QG, UK
- 2Rare and Imported Pathogens Laboratory, Public Health England, Porton Down, UK
- Correspondence to: I Cropley iancropley{at}nhs.net
What you need to know
Zika virus, transmitted by mosquitoes, has spread rapidly recently in the Americas, and it is likely to spread further in the presence of Aedes mosquitoes
Zika virus infection causes either a mild illness with fever, rash, conjunctivitis, arthralgia, and myalgia, or it may be subclinical
Some Brazilian regions experiencing outbreaks of Zika virus infection have reported an apparent increase in congenital microcephaly. Some countries experiencing outbreaks have reported an increase in post-infective neurological syndromes, particularly Guillain-Barré syndrome. An association with Zika virus has yet to be confirmed
The situation is changing rapidly, and up to date advice must be sought about travel to affected areas, particularly with regard to pregnancy and sexual transmission
Zika virus is spreading rapidly in the Americas. The virus was identified in the late 1940s in Africa but was first confirmed in Brazil in May 2015. It has since been identified in more than 27 countries and territories in the region.1 2 Spread to the Americas was predicted because of the abundance of the mosquito vector, Aedes aegypti.3 4 5 6 Clinicians worldwide need to be aware of Zika virus infection owing to international travel and the presence of another potentially competent mosquito vector (Aedes albopictus) in North America and southern Europe. Some Brazilian regions experiencing outbreaks of Zika infection have reported an apparent increase in congenital microcephaly and post-infective neurological syndromes, particularly Guillain-Barré syndrome (see boxes 1 and 2).2 The association of these conditions with Zika virus infection is currently unproved and is under investigation. On 1 February 2016, the World Health Organization declared the recent cluster of microcephaly and other neurological disorders reported in Brazil, following a similar cluster in French Polynesia in 2014, a public health emergency of international concern.7 If Zika virus infection is confirmed to cause congenital microcephaly, this could lead to a large international burden of infant neurological morbidity. Zika virus infection should be considered in people presenting with compatible symptoms who have recently returned from countries where outbreaks of the infection are occurring. This review provides up to date information at the time of publication on Zika virus, its evolving epidemiology, how to recognise its clinical presentation, possible complications, and how to confirm the diagnosis.
Box 1: Case reports of fetal Zika virus infection
Zika virus detected by polymerase chain reaction (PCR) in amniotic fluid in two infants with microcephaly in north east Brazil15
Serological evidence of past Zika virus infection identified in Hawaii in a baby with congenital microcephaly born to a mother who resided in Brazil during the pregnancy57
In north east Brazil, Zika virus detected in brain tissue of two neonates with microcephaly who died within 20 hours of birth, and in the placental tissue of two early miscarriages. All four mothers reported illness compatible with Zika virus infection in the first trimester of pregnancy58
Zika virus detected by PCR in fetal brain tissue of terminated pregnancy of microcephalic fetus in Slovenia. Mother had been in north east Brazil in the first trimester of pregnancy59
Box 2: Reported increase of Guillain-Barré syndrome and other post-infective neurological syndromes
Reported increases in Guillain-Barré syndrome (GBS) are associated with the Zika virus outbreaks in Brazil, El Salvador, Colombia, Suriname, and Venezuela2
50 out of 66 (76%) GBS cases in Venezuela indicated a clinical history consistent with Zika virus infection, with Zika virus detected by polymerase chain reaction (PCR) in three patients2
1708 GBS cases registered in Brazil in 2015, a 19% increase, compared with 1439 the preceding year. In 42 people with confirmed GBS, 26 (62%) gave a history of symptoms consistent with Zika virus infection2
Of 42 people with confirmed GBS in French Polynesia, 37 (88%) reported an illness consistent with Zika virus infection. All had serological evidence of flavivirus infection2 52
In two people with GBS in Martinique, Zika virus infection was confirmed by positive urine PCR60
Sources and selection criteria
We searched Medline and Embase for published articles on Zika virus using the term “Zika”, and checked the bibliographies of all full text articles retrieved. For unpublished information, we searched ProMed. We also accessed key information from national and international public health websites, including the European Centre for Disease Prevention and Control (http://ecdc.europa.eu/), the World Health Organization (www.who.int/), and the Pan American Health Organization (www.paho.org/), and searched the bibliographies of all alerts and risk assessments issued by these organisations.
What is Zika virus?
Zika virus is an arbovirus (arthropod borne virus). It is a member of the Flaviviridae family, genus Flavivirus, which includes dengue, yellow fever, and West Nile viruses. It was first identified in the Zika forest near Kampala, Uganda in rhesus macaques in 1947.8
Zika virus is a single stranded RNA virus with two major lineages: Asian and African.4 9 10 In Africa, Zika virus is thought to have been largely maintained in a cycle involving transmission between non-human primates (such as monkeys and apes) and mosquitoes, with humans as occasional unintentional hosts.11 12 In areas outside Africa, however, humans have probably become the main host.3
Few complete Zika virus genome sequences are available, and to date only two are from the current South American epidemic. Phylogenetic analysis of a Suriname Zika virus indicates that it belongs to the Asian genotype. It is most closely related to the strain that was circulating in French Polynesia in 2013, sharing more than 99.7% and 99.9% of nucleotide and amino acid identity, respectively.13 This finding is consistent with analysis of envelope gene sequences from Brazilian patients.14 15 A mutation in the Asian lineage may have led the virus to adapt to the human (as opposed to non-human primate) host.16
Until recently, Zika virus was less of a research priority than other flaviviruses, as it was not thought to be of public health importance. Limited literature exists on the pathogenesis of the Zika virus to help understand the clinical disease spectrum and to target treatments to minimise or prevent tissue damage.17 18 Zika virus replicates readily in skin immune cells, and a large number of receptors are able to mediate entry of the virus into cells.18 Studies on the capability of the virus to replicate in neuronal cells are warranted to further investigate the link with neurological disorders.
Epidemiology
Between the first isolation of Zika virus in monkeys in 1947 until 2007, reports of human cases were rare and sporadic.8 19 20 Evidence on the extent of human infection was based mainly on serological studies and, in some cases, isolation of the virus.19 21 22 23 24 25 Viral isolation suggested a wide distribution in Africa and South East Asia, although no epidemics were observed.
In 2007 an outbreak caused by a strain of Asian lineage occurred on the island of Yap, an island state of the Federated States of Micronesia.3 4 Estimated cases affected in this and subsequent outbreaks to date are probably imprecise, given the incomplete laboratory confirmation and the similarities in clinical presentation of Zika virus with other arbovirus infections present throughout the tropics. In Yap, 49 confirmed and 59 probable cases (defined according to strict serological criteria or RNA detection by reverse transcription-polymerase chain reaction) were identified over a four month period.3 On the basis of one serological test, an estimated 73% of the island’s population were infected over three years.
A further outbreak occurred with a closely related Asian lineage strain in French Polynesia in 2013 in which 294 cases were confirmed by RNA detection over a 10 week period.26 27 Locally acquired cases (people with no history of travel to known endemic areas within the recognised incubation period) on Easter Island in 2014 marked the first arrival of Zika virus in the Americas.28 This was followed in May 2015 by confirmation of cases in north east Brazil, where again the Zika virus sequence belonging to the Asian lineage was found.14 29
Zika virus is new in the Americas and there is no immunity within the population. Its rapid spread and large number of cases mirrors that of the recent arrival of the chikungunya virus in the Americas in 2013.
Because most people with Zika virus infection may not present for medical attention, estimating the total number of infected cases from the numbers of clinically suspected and laboratory confirmed cases is problematic. Estimates are influenced by the criteria used for definition of a suspected case and by assumptions made about the proportion of subclinical infections. Brazilian authorities estimate that around 1.5 million cases of Zika virus infection have occurred since the outbreak began.2 Colombia reported local transmission in October 2015, with now more than 25 000 suspected cases. Figure 1⇓ shows the areas with confirmed locally acquired cases in the past nine months.2
Fig 1 Areas of locally acquired Zika virus infection, June to February, 2016. Adapted from World Health Organization situation report, 19 February 20162
How is the virus transmitted?
The key Zika virus vector is thought to be the daytime biting (indoors and outdoors), urban dwelling Aedesaegypti mosquito. Evidence to support this comes from detection of the virus in wild A aegypti and by experimental transmission in rhesus monkeys.30 31 32 Following laboratory feeding of Aedes albopictus mosquitoes with Zika virus infected blood, the virus has been demonstrated in mosquito saliva, suggesting these mosquitoes may also transmit the virus.33 34
Presumptive sexual transmission has been reported in two cases.35 36 Isolation of virus in semen 17 days after a clinical diagnosis of acute infection supports potential sexual transmission, as does the detection of Zika virus RNA in semen 62 days after the onset of symptoms.37 38
Zika virus was detected in approximately 3% of asymptomatic blood donors during the French Polynesian outbreak,39 suggesting that transmission might be possible through infected blood and blood products.
Evidence implies transplacental transmission and perinatal transmission during delivery, with Zika virus RNA being found in amniotic fluid15 and in paired blood samples taken from newborn infants and mothers.40
There is currently no evidence to support transmission via contact with saliva, urine, or respiratory droplets.
How does Zika virus present?
Zika virus infections seem either to be subclinical (possibly in as many as 80% of infections) or to cause a mild illness after an incubation period of three to 12 days. Symptoms, which last for approximately two to seven days include fever, conjunctivitis, arthralgia, myalgia, and widespread rash, which may be itchy. Headache, retro-orbital pain, peripheral oedema, and gastrointestinal disturbance have also been observed.3 41 42 43
Only one study has examined the proportion of infections that produce symptoms. A serological survey during the Yap outbreak found that only 19% of participants with IgM antibodies against Zika virus reported rash, joint pains, or conjunctivitis that were probably attributable to Zika virus infection. Whether the remaining infected participants experienced any other symptoms was not reported.3 The proportion of infected people who experience no symptoms is not known. Observation of Zika viraemia in 31 French Polynesian blood donors who reported no symptoms, during or after blood donation, suggests that asymptomatic infection does occur.39
Shock and haemorrhage occur with other flaviviruses such as dengue, but they have not been documented in Zika virus infection. Severe acute illness seems to be rare. Fewer than 10 possible Zika related deaths have been reported in adults, and an additional three deaths from Guillain-Barré syndrome have occurred in individuals who had symptoms of Zika infection.44 45
Is there evidence for an association between infection and complications?
Current epidemiological data suggest spatial and temporal links with the Zika virus epidemic and congenital microcephaly. These are supported by case reports of detection of the virus from amniotic fluid or the brain tissue of affected fetuses. Robust epidemiological studies with clear definitions of microcephaly are under way to test whether any association with Zika virus infection can be confirmed.
Microcephaly usually results from abnormal brain development (see box 3 for causes of microcephaly). There is no internationally accepted definition of microcephaly. The Brazilian Ministry of Health is now using a definition of head circumference of less than 2 standard deviations (3 standard deviations for severe microcephaly) below the mean for sex and gestational age at birth.46
Box 3: Causes of microcephaly
Chromosomal and genetic abnormalities
Craniosynostosis (premature fusion of cranial sutures)
Fetal infection during pregnancy (eg, rubella, toxoplasmosis, cytomegalovirus, varicella, herpes simplex)
Exposure to drugs, alcohol, and toxins (eg, cocaine, antiepileptic drugs, lead or mercury intoxication)
Severe maternal malnutrition
Over 85% of the cases of microcephaly from November 2015 have been reported from the state of Paraíba, north east Brazil. Reported cases of microcephaly increased from 5.7 per 100 000 live births in 2010 to 99.7 per 100 000 live births from November 2015 to January 2016.47 It is not yet clear whether this is a true increase, an increase in severe cases, or an increase in ascertainment. Colombia, where Zika virus has been present since October 2015, has reported over 30 000 cases of Zika virus infections, more than 5000 of which were in pregnant women. As yet, there are no reports of associated cases of microcephaly.48
From November 2015 to 13 February 2016, 5280 suspected cases of microcephaly and/or central nervous system malformation, including 108 deaths, were reported by Brazil—1345 of these have been investigated further: 837 of the 1345 did not have microcephaly, 421 had radiological findings such as cerebral calcifications compatible with a congenital infection, and 41 had laboratory confirmed Zika virus infection.2
A retrospective review of birth data in French Polynesia showed 18 cases of central nervous malformations in children born between March 2014 and May 2015, including nine cases of microcephaly, compared with the previous national annual average of none to two cases.2
How is Zika virus infection diagnosed?
Clinical
The clinical picture of Zika virus infection is similar to that of other mosquito borne viruses such as dengue and chikungunya, which often co-circulate in the areas where Zika virus is endemic.
The Pan American Health Organization of WHO has issued a provisional case definition for suspected acute Zika virus infection, intended for use in countries with ongoing local transmission (see box 4).49
Box 4: Provisional case definition of suspected acute Zika virus infection. Pan American Health Organization49
Rash or increase in body temperature (>37.2°C), with any of the following not explained by other conditions:
Arthralgia or myalgia
Non-purulent conjunctivitis
Conjunctival hyperaemia
Headache
Malaise
The differential diagnosis of Zika virus infection is wide. Diagnosis is guided by history (countries of travel, sexual contacts, and contact with other cases of infection) and examination. In addition to dengue and chikungunya, other diagnoses that should be considered include HIV seroconversion, measles, scarlet fever, rickettsial infection, leptospirosis, parvovirus, enterovirus, rubella, and secondary syphilis. The symptoms and clinical signs do not have sufficient positive or negative predictive value, and therefore laboratory testing is needed for reliable diagnosis.
Laboratory testing
Definitive diagnosis is based on detection of Zika virus RNA in blood (serum or, ideally, EDTA treated plasma) and other body fluids by polymerase chain reaction (PCR) (table 1⇓).
Diagnostic tests for Zika virus
After the acute phase, diagnosis by antibody detection in serum samples is compromised by considerable cross reactivity with antibodies to other flaviviruses; false positive results can be seen with past dengue infection or previous yellow fever vaccination.52
How is Zika virus infection managed?
There is currently no vaccine against Zika virus, nor specific antiviral for the treatment of Zika virus. Treatment is symptomatic, although it is not known what agents are optimal for treating the fever, itch, and arthralgia. Minimisation of the chance of mosquito bites is advised by wearing long sleeves and trousers and using mosquito repellents.54 Specific travel advice is dealt with in the accompanying article.55 56
Vector control by insecticides and removal of small pools of stagnant water, the breeding sites for Aedes, is being instituted on a local level. Trials of the release of irradiated sterile mosquitoes are being considered by WHO.
Key research questions
Are the reported epidemiological links between Zika virus infection in pregnancy, fetal microcephaly, other birth defects, and Guillain-Barré syndrome borne out by rigorous studies?
Is there a causal relation between Zika virus infection in pregnancy and fetal microcephaly?
What is the risk of fetal abnormality following Zika virus infection in pregnancy?
Can asymptomatic Zika virus infection result in fetal abnormality?
Can serological testing reliably exclude recent Zika virus infection in pregnant women?
What is the optimal approach to prenatal diagnosis of fetal infection and disease?
What is the optimal approach to assessment of neonates born to women with suspected but unconfirmed Zika virus infection in pregnancy?
How long does infectious virus persist in semen?
Does infection confer lasting immunity?
Can a safe and effective vaccine be developed?
How were patients involved in the creation of this article?
The BMJ did not ask the authors to involve patients in the creation of this article.
Additional educational resources
Resources for healthcare professionals
Public Health England (www.gov.uk/guidance/zika-virus)—up to date UK guidance, epidemiology, and clinical advice
Royal College of Obstetrics and Gynaecology (www.rcog.org.uk/en/news/qas-related-to-zika-virus-and-pregnancy/)—guidance on Zika virus infection in pregnancy in Q&A format
World Health Organization (www.who.int/csr/disease/zika/en/)—factsheets, epidemiology updates and weekly situation reports, and overview of global response
Pan American Health Organization (www.paho.org/hq/index.php?option=com_content&view=article&id=11599&Itemid=41691&lang=en)—epidemiological updates, current and previous epidemiological alert documents, detailing the background to the current situation
European Centre for Disease Prevention and Control (http://ecdc.europa.eu/en/healthtopics/zika_virus_infection/Pages/index.aspx)—epidemiological updates and risk assessments of the possible association with Zika virus and neuropathologies; mosquito maps; links to peer reviewed publications
Centers for Disease Control and Prevention (www.cdc.gov/zika/index.html)—summarises PAHO information (see website above), US health advice on Zika virus, links to publications
Resources for patients
Travel Health Pro (travelhealthpro.org.uk/zika-virus-update-and-advice-for-travellers-including-pregnant-women/) or fitfortravel (www.fitfortravel.nhs.uk/advice/disease-prevention-advice/zika-virus-infection.aspx)—summary of background information and focus on travel and prevention advice
NHSChoices (www.nhs.uk/Conditions/zika-virus/Pages/Introduction.aspx)—overview of Zika virus infection, the current situation, and links to advice on travel
European Centre for Disease Prevention and Control (http://ecdc.europa.eu/en/healthtopics/zika_virus_infection/zika-outbreak/Pages/Frequently-Asked-Questions.aspx)—key information summarised in a frequently asked questions based approach, with useful links
Footnotes
Contributors: All authors carried out the literature search and wrote and reviewed the article. IC is the guarantor.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following: none.
Provenance and peer review: Commissioned; externally peer reviewed.

